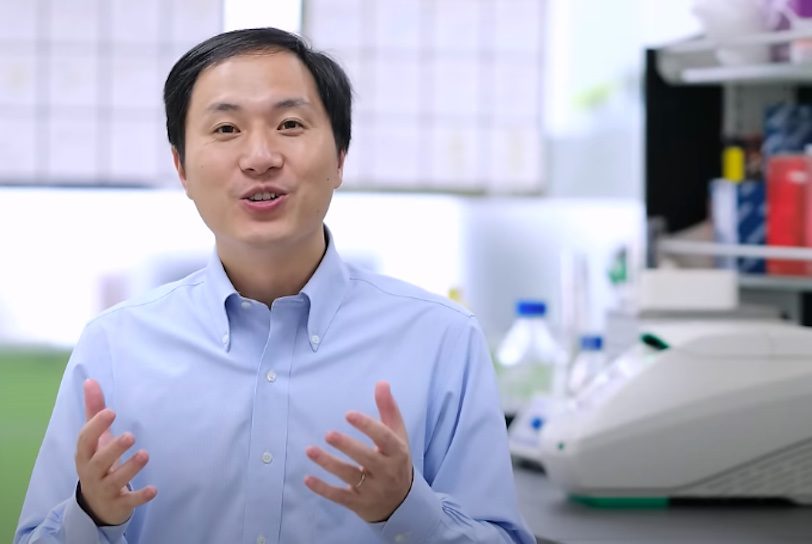
Controversial Chinese scientist He Jiankui faced consequences after asserting in November 2018 that he employed CRISPR gene editing technology to produce a pair of HIV-resistant newborn twins. He now intends to utilize a different technique, known as “base editing,” to prevent Alzheimer’s disease, a degenerative brain ailment that impacts 55 million individuals globally and can lead to dementia and death.
At present, U.S. law and universal medical ethics dictate that gene editing should solely apply to laboratory animals for assessing its safety for humans. However, if He succeeds, his research could lead to a breakthrough in preventing other incurable diseases.
In November 2018, He disclosed that his research team utilized a gene editing approach called CRISPR to modify the sperm cells of men with HIV. CRISPR eliminated mutations in the DNA of sperm cells that cause HIV and introduced a chemical combination providing HIV resistance. The modified sperm cell was then used to fertilize an egg from an HIV-negative woman, resulting in the birth of HIV-resistant twin girls named Lulu and Nana.
Despite He's ongoing monitoring of the girls’ well-being, genetic scientists worldwide condemned him for “unethically” employing untested technology to modify the DNA of two infants who could not consent (although their parents did). Critics noted that gene editing can lead to unintended DNA mutations resulting in unforeseen pain, illnesses, and death.
In December 2019, a Chinese court sentenced He to three years in prison and fined him 3 million Chinese yuan (about $434,000). He also supposedly faces a lifetime ban from genetic research. according to Time magazine.
Nevertheless, He says still plans to use a different gene editing method, known as “base editing,” to impede the progression of Alzheimer’s in a lab mouse. If successful, it would likely require government permits, ethical approvals, and numerous experimental trials before being authorized for testing on human patients.
Nevertheless, a closer examination of gene-editing technology provides insight into how medical researchers may potentially use it to cure many presently incurable diseases.
What is CRISPR and how is it different from “base editing”?
CRISPR, short for “clustered regularly interspaced short palindromic repeats,” is essentially a cut-and-paste tool for editing DNA. DNA, the chemical strands inside our cells, can impact our physical traits and susceptibility to certain diseases.
CRISPR employs a “guide RNA” to identify specific chemical mutations in DNA responsible for hereditary diseases. It then uses a “Cas9 protein” to cut a DNA strand, enabling scientists to modify the strand or introduce new chemical combinations to prevent the development of these diseases.
Base editing resembles CRISPR in its use of a guide RNA and a Cas9 protein, but instead of modifying or replacing DNA strands, the Cas9 protein utilizes an attached enzyme to alter individual chemicals one by one in a DNA strand.
It may be useful to see CRISPR and base editing as two different types of “spell-checkers” that can find misspellings (or disease-causing mutations) in DNA strands. CRISPR removes and replaces entire words all at once, while base editing alters individual letters inside of words one at a time.
Because CRISPR cuts and inserts completely new chemical combinations into DNA, it sometimes leads to “indels,” incorrect insertions and deletions that can accidentally create harmful DNA mutations. Since base editing changes individual chemicals in a DNA strand, it’s considered more precise and less likely to lead to harmful mutations.