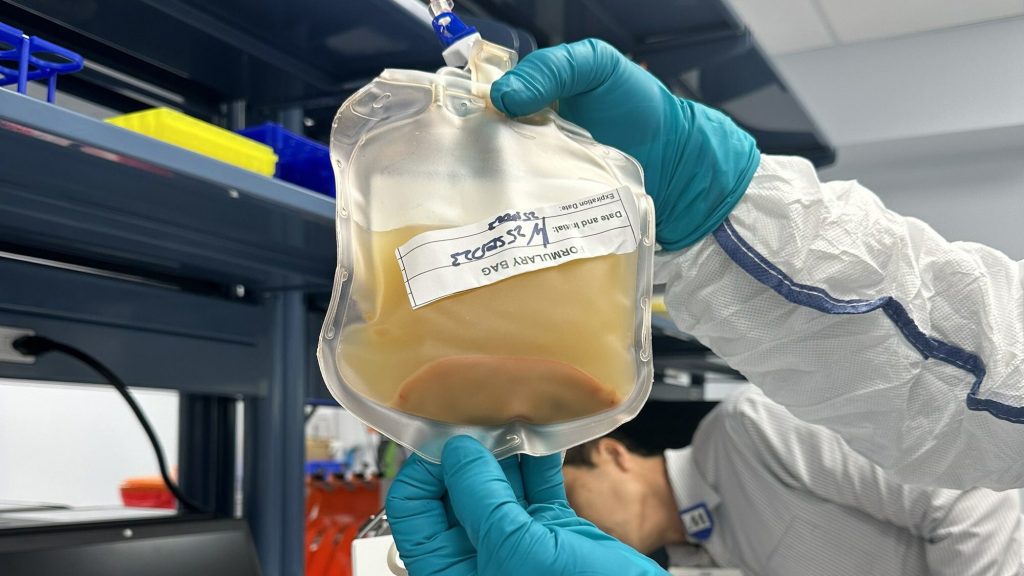
A team of scientists is trying to grow a new liver inside a person using an experimental treatment. liver within a person's body using an experimental treatment. lymph nodes. While this may sound like something from a science fiction story sounds far-fetched, a biotech company called LyGenesis announced that a volunteer has been given an injection of liver cells from a living donor. This injection could transform one of their lymph nodes into a functioning liver.
This experimental procedure happened in Houston on March 25 as part of a Phase 2a clinical trial. It is to test this treatment on 12 adults with end-stage liver disease. liver disease so severe it cannot be reversed end-stage liver disease (ESLD). This condition occurs when the liver is severely damaged, mainly due to chronic liver disease or sudden liver failure. Over 50,000 people in the US die from chronic liver disease annually.
Patients with ESLD usually need a liver transplant, but about 10,000 people are currently waiting for one in the US . In 2021, the US conducted a record 9,234 liver transplants, according to the federal government’s Scientific Registry of Transplant Recipients. LyGensis hopes this procedure will create enough liver tissue growth so patients won’t need a transplant.
[Related: Swiss researchers kept a donor liver healthy for an impressive 68 hours.]
LyGenesis co-founder and CEO Dr. Michael Hufford stated, “This therapy has the potential to be a significant milestone in regenerative medicine by helping patients with ESLD grow new functional ectopic livers in their own body.” said in a statement. He also mentioned that if the study is successful and FDA approval is obtained, one donated liver could potentially help dozens of ESLD patients, which could address the imbalance between organ supply and demand in favor of patients.
The technique has been in development for more than a decade. for over ten years. It involves taking liver cells from a donated organ and injecting them into the lymph nodes found throughout the body. The aim is for the liver cells to multiply, grow, and form blood vessels within the lymph nodes. This procedure targets a set of lymph nodes in the abdomen that are linked to the liver through a system of veins.
According to MIT Technology Review, LyGenesis has tested this method on mice and pigs, finding that the cells can thrive and create an additional liver capable of taking over the function of the animal’s failing organ. In a study from 2020, the chief scientific officer of LyGenesis and University of Pittsburgh pathologist Dr. Eric Lagasse published a found that the pigs regained their liver function following the injections. They also observed that the more severe the damage to the original liver, the larger the second liver grew, suggesting that the pig’s body may prioritize the healthier tissue and give the new liver more responsibilities. The doctors inserted a thin, flexible tube through the patient's throat and digestive tract during the trial. They used an ultrasound to locate one of the target lymph nodes and placed 50 million liver cells into it.
According to . They then utilized an ultrasound to locate a target lymph node and injected 50 million hepatocytes into it. Wired. They then used ultrasound to locate one of the target lymph nodes and injected 50 million hepatocytes into it.
[Related: The first-ever gene-edited pig kidney transplant has been completed by surgeons..]
“LyGenesis’ cell therapy platform represents a remarkable potential business opportunity and could be a game-changer for chronic liver failure patients without access to a donor liver,” stated LyGenesis investor Justin Briggs from Prime Movers Lab stated in a statement. “Their use of an endoscopic ultrasound as a low risk and low cost method of cell therapy administration is another way this innovative technology could offer patients access to life-saving treatments and tackle complicated medical issues by revolutionizing transplant medicine.”
The findings will not be available for a few months and the team will be observing how many cells are needed to grow a liver that is big enough to filter blood and produce bile. If it works, it could signify a significant change for the treatment of liver disease, which impacts approximately 4.5 million people in the United States.