For individuals with spina bifida, paralysis, and various bladder conditions, knowing when to take a bathroom break can be difficult. To help reduce the stress, researchers at Northwestern University have created a sensor device that connects to the outside of the bladder, allowing it to detect when it's full in real time. Using Bluetooth technology, the device then sends its data to a smartphone app, enabling users to monitor their bodily functions with much less discomfort and uncertainty.
The new tool, described in a study released today in the Proceedings of the National Academy of Sciences (PNAS), is not just intended to prevent incontinence problems. The inability to sense bladder fullness goes beyond inconveniences—for millions of Americans with bladder issues, not knowing when to use the bathroom can lead to additional organ damage such as frequent infections and kidney damage. To address these issues, the new medical device mimics the bladder’s natural flexibility.
[Related: This drug-delivery soft robot could help address the scarring problem with medical implants.]
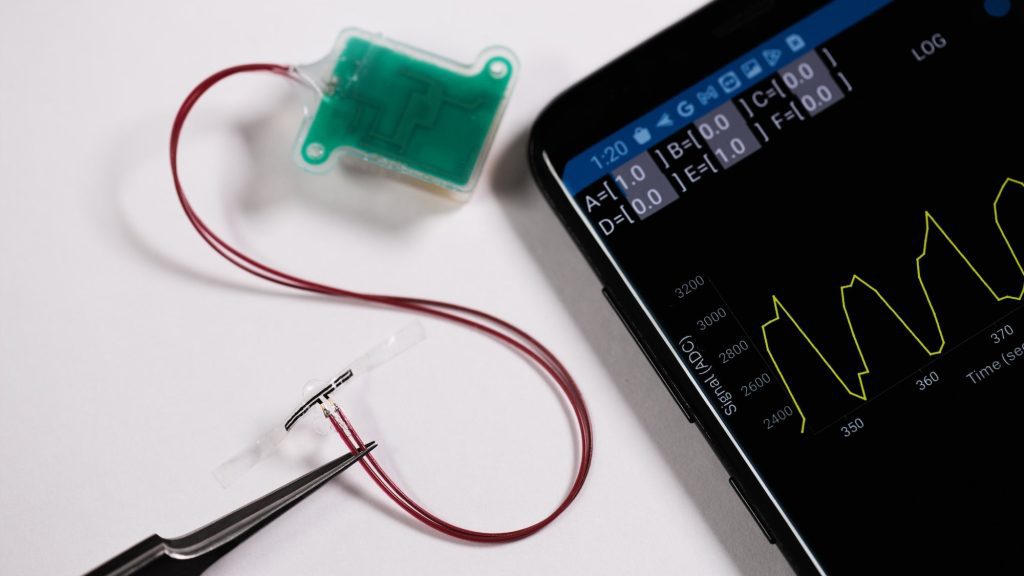
“The major advancement here lies in the creation of very soft, extremely thin, stretchable strain gauges that can gently wrap around the outer surface of the bladder, without imposing any mechanical limitations on its natural filling and emptying actions,” John Rogers, study co-lead and professor of material sciences and biomedical engineering at Northwestern University, stated in a press release.
As the bladder fills with urine, its expansion stretches out the sensor material, which then wirelessly sends data to a patient’s smartphone app. This also works as the organ contracts after urination, providing users with real-time data throughout the day's ups and downs. In small animal lab tests, the battery-free device was able to accurately monitor a bladder for 30 days, while the implant remained effective in non-human primates for up to 8 weeks.
“Depending on the situation, we can design the technology to remain permanently inside the body or to safely dissolve after the patient has fully recovered,” regenerative engineer and study co-lead Guillermo Ameer expressed on Monday.
The researchers think their device could decrease the need for uncomfortable, infection-prone catheters, and also reduce the requirement for more invasive, in-patient bladder monitoring procedures. But why stop there?
The team is also testing a separate, biodegradable “patch” utilizing a patient’s own stem cells. Known as a pro-regenerative scaffold (PRS), the new material also expands and contracts along with the bladder’s movements while promoting the growth of new organ cells. New tissue remains in place as the patch dissolves, facilitating faster, more effective healing possibilities. Researchers aspire to one day integrate their PRS work with their wireless monitoring sensors.
“This work brings us closer to the possibility of smart regenerative systems, which are implantable pro-regenerative devices capable of examining their surroundings, wirelessly reporting those findings outside the body… and allowing for prompted or programmed responses to adjust and enhance device performance or safety,” said Ameer.
To have even better restored functionality, the team thinks that their sensors could eventually include more technology to prompt urination using the smartphone app. Altogether, these three medical advances might one day provide a much less irritating, comfortable, and efficient treatment for patients with bladder problems.